How To Prevent Errors In Medical Record Documentation
Accurate and comprehensive medical records are vital for the healthcare industry. They support high-quality patient care, effective health research, and efficient healthcare operations. However, mistakes in documenting medical information can cause significant problems. These errors can lead to misunderstandings among healthcare teams, wrong treatment decisions, and even legal troubles.
This is why it’s crucial to take proactive steps to prevent these errors and ensure that medical records are concise and reliable. Some of these include the following:
- Recognize Common Documentation Errors
The first crucial step in addressing medical record documentation errors is recognizing the common ones. Errors often include:
- Incorrect patient information such as misrecorded medical histories or wrong patient demographics
- Incomplete records that might lack vital data like allergy information and medication lists
- Mislabelled files such as those with incorrect patient name labels or misplaced test results
- Inappropriate alteration of records
In addition, illegible handwriting and inconsistent use of terminology may result in misunderstandings. Technologies and services that convert Word to PDF make maintaining clear, standardized records easier.
- Promote The Use Of Standardized Forms And Templates
A major issue in medical record documentation that can lead to errors is the lack of a uniform system for recording and presenting information. In many healthcare settings, practitioners may use their own unique methods for recording data, leading to inconsistencies, misinterpretations, and, subsequently, errors.
To mitigate this, healthcare organizations should actively promote standardized forms and templates. One of their primary benefits is that they ensure clear communication among healthcare providers. They establish a shared understanding of what data needs to be documented and where it should be located within the record.
This uniformity aids in quick information retrieval, fostering more efficient and effective patient care. This is especially helpful in terms of precision health, which focuses on personalizing healthcare to fit the individual needs of every patient.
Moreover, standardized forms and templates often have built-in prompts and checkboxes that reduce the chances of omitting critical information. For example, a template for patient history might include specific fields for allergies, past surgeries, and chronic illnesses. These prompts ensure that healthcare providers don’t overlook essential information during documentation.
However, it’s important to keep in mind that while standardization is crucial, flexibility is equally essential. Medical record forms and templates should allow for individualized patient care notes where necessary. This way, healthcare organizations can provide more personalized care while still maintaining a high level of consistency in their documentation.
- Implement Robust Training Programs
After recognizing the potential pitfalls, implement robust training programs. In addition to traditional documentation methods, these programs could also enhance the adaptability and accessibility of medical records.
Ensuring all healthcare providers understand the importance of accurate and complete documentation can significantly reduce the occurrence of errors. Furthermore, ongoing education sessions can serve as useful refreshers on proper documentation procedures.
- Leverage Electronic Health Records
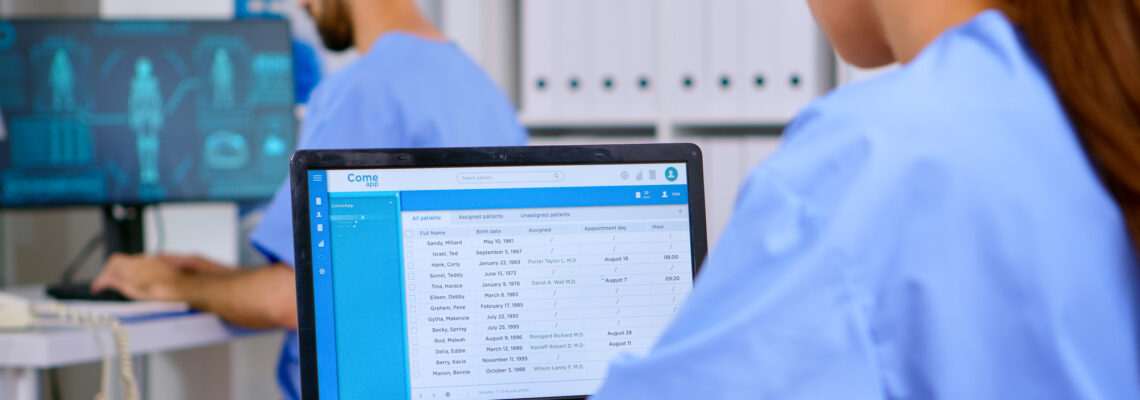
Moving on to more technologically advanced methods, consider leveraging Electronic Health Records (EHRs). These digitally stored records can help to ensure that all patient data is legible, organized, and easily accessible, which can be vital in preventing inaccuracies or omissions that can occur with manual paperwork.
One of the most significant benefits of EHRs is the decrease in duplication of records. In a traditional, paper-based system, it’s easy to duplicate or create multiple versions of a patient’s information, leading to confusion and potentially significant errors in treatment.
EHRs prevent this by providing a single, unified record for each patient. Any healthcare provider with access to the EHR system can view or update a patient’s record, ensuring that everyone uses the same details.
Error checking is another crucial feature of most EHRs. These systems are programmed to automatically flag potential errors or inconsistencies in the data. For example, EHRs might alert when a prescribed medication interacts negatively with another drug that the patient is taking.
They may also spot when a prescribed treatment might be contraindicated due to a patient’s pre-existing conditions or known allergies. Such systems might also prompt healthcare providers to complete essential fields, reducing the likelihood of missing critical patient data.
Despite the significant role of EHR systems in reducing medical record errors, the quality of data entry remains critical. Healthcare providers should enter only accurate and comprehensive information into the system. Training and guidelines on proper EHR use are also vital to maximize their full potential in medical record documentation.
- Establish Regular Auditing Procedures
While these preventive measures can significantly decrease the occurrence of errors, it’s essential to have mechanisms in place to catch any mistakes that do slip through. With that in mind, establishing regular auditing procedures is beneficial.
Auditing systematically examines and evaluates records and the overall recording process. The aim is to detect inconsistencies, discrepancies, and potential areas for improvement, enabling the healthcare institution to maintain an accurate and reliable record-keeping system.
These auditing procedures can be executed on a routine basis, depending on the size and requirements of the medical facility. The key is striking a balance between regular checks for sustained accuracy and avoiding disruption of healthcare professionals’ workflow with excessive audits.
Regular audits uncover errors and reveal trends indicating potential systemic issues in the documentation process. Such insights are vital for improving the quality of healthcare delivery, patient safety, and the overall efficiency of the healthcare institution. It’s also beneficial for meeting regulatory requirements, demonstrating transparency, and maintaining trust among patients and stakeholders.
- Encourage Open Communication
Open communication is critical for reducing medical record documentation errors. Here are some strategies to encourage this:
- Foster A Non-Punitive Culture: Create an environment where staff isn’t afraid to admit or point out errors, viewing them as learning opportunities instead of punishable offenses.
- Hold Regular Meetings And Training: Use these to discuss common mistakes, suggest solutions, and reinforce the importance of accurate documentation for patient safety.
- Institute A Feedback Mechanism: Allow staff to give and receive constructive feedback on their record-keeping practices, helping identify areas for improvement.
- Highlight The Importance Of Communication In Patient Safety: Emphasize that open communication is a key component of patient safety, motivating staff to actively discuss and prevent errors.
Promoting open communication can help healthcare organizations reduce medical record documentation errors, thereby enhancing patient care quality.
Conclusion
Reducing medical record documentation errors isn’t just a matter of meeting standards or avoiding legal issues. It’s about committing to a higher purpose—safeguarding patient safety, enhancing quality care, and driving effective healthcare delivery. By diligently following the methods outlined above, healthcare providers not only minimize documentation errors but also ensure that they honour their commitment to their patients.


